
patients with limited skin involvement (BSA ≤3 palms) considered their current psoriasis symptoms to be more severe than what their BSA would suggest 1,*,†

85% of patients with limited skin involvement reported feeling “embarrassed or self-conscious because of their skin” 2,‡
*Based on the UPLIFT survey, a multinational online survey conducted from March 2 to June 3, 2020, including adult patients (≥18 years of age) who reported that they had been diagnosed with plaque psoriasis and/or psoriatic arthritis by a healthcare professional. 1006 patients were surveyed in the United States. †In the UPLIFT survey, mild disease was defined as with ≤3 palms of affected area and moderate disease was defined as 4-10 palms of affected area. ‡Based on an online US cross-sectional survey among 175 adult patients on prescription topicals for mild to moderate plaque psoriasis (BSA ≤10%).
Patients with psoriasis in one or more special areas (such as the scalp, nails, or genitals) reported that their plaques may get in the way of work or studying 3
Among plaque psoriasis patients with limited skin involvement (BSA ≤3 palms; n=1927) and manifestations in ≥1 special area, 60% rated their disease to be moderate or severe 3,§


51% of those patients were receiving either no treatment, or were being treated with topicals alone 3,§


§Based on the UPLIFT survey.
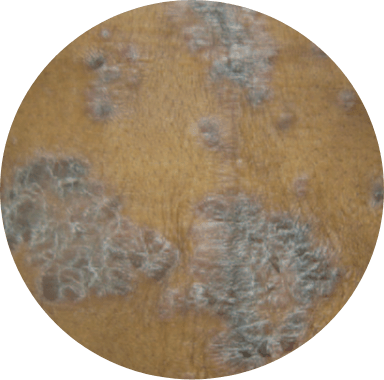
Even if a patient has limited BSA, psoriasis may feel severe when it occurs in special locations like the scalp. 4-8
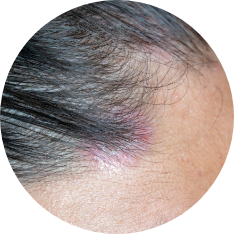
Up to 97% of patients with scalp psoriasis report that the condition interferes with their daily lives 9

higher risk of developing psoriatic arthritis in patients with scalp psoriasis 10,*
*In a population-based setting, among 1,633 patients first diagnosed with psoriasis, 97 subjects were diagnosed with psoriatic arthritis according to the CASPAR criteria. Cox proportional hazard models were used to identify predictors of psoriatic arthritis within the psoriasis cohort.

“My scalp was raw all the time. It was all kinds of horrible.”
- JENNIFER
Not an actual patient.
Quote and profile inspired by a real patient story.
Nail psoriasis is particularly difficult to treat, and it is often a persistent condition. 11

50% of patients with psoriasis experience fingernail changes 11

There is a ~3X higher risk of developing psoriatic arthritis in patients with nail psoriasis 10,†
†In a population-based setting, among 1,633 patients first diagnosed with psoriasis, 97 subjects were diagnosed with psoriatic arthritis according to the CASPAR criteria. Cox proportional hazard models were used to identify predictors of psoriatic arthritis within the psoriasis cohort.
Though genital manifestations can trouble patients a great deal, many may be reluctant to discuss it with a healthcare provider. 12,13
46% of psoriasis patients have not discussed their genital psoriasis with a physician due to embarrassment 12

82-100% of patients
with genital psoriasis may experience itch 13
>2/3 patients with genital psoriasis are undertreated, having never applied treatment to their genital regions 14
In psoriasis, itch is a primary source of discomfort that can impact one’s well-being.
60%-96% of
psoriasis patients experience itch.
8

“I really had no idea how to manage [the itch]. That was the worst part…I [felt like I] was ripping out chunks of my skin.”
- JENNIFER
Not an actual patient.
Quote and profile inspired by a real patient story.
43% of psoriasis patients report itch as their most bothersome skin symptom 15,‡
5X the proportion of patients vs dermatologists cite itching as the most important factor of contributing to disease severity (38% vs 7%) 16,§
‡MAPP was a population-based survey of 3,426 patients and 781 physicians in North America and Europe that aimed to determine the impact of psoriasis and psoriatic arthritis on HRQoL and to identify unmet treatment needs. §The MAPP survey provided context on the impact of disease and treatment on patient’s daily life from both the patient and physician perspectives. The physician survey included dermatologists (n=391) and rheumatologists (n=390).

“After 3 topicals, I’m still struggling with itch. Why do we keep trying the same thing?”
- EVAN
…But while topicals are often efficacious where applied on the skin, plaque psoriasis is a chronic systemic disease2,17
Despite many therapeutic options, many patients with limited skin involvement receive no therapy or are treated with topicals alone.3
But topical therapy only addresses the skin area where it is applied, not the underlying systemic inflammation.3

60% still experienced itching18

92% had nail psoriasis that persisted18

~76% had scalp psoriasis that persisted18

48% had no BSA reduction after a mean duration of 6.9 months on topical therapy18
**Based on a real-world study of 304 adult systemic-naïve patients with mild to moderate (BSA ≤10%) plaque psoriasis from a survey of physicians; patients still affected by nail psoriasis (n=24/26), scalp psoriasis (n=120/158), and itching (n=125/207). Data were drawn from the 2017 to 2018 Adelphi Psoriasis Disease Specific Programme. Most patients were receiving a generic topical steroid formulation at the time of consultation (72.7%, n=221); 23.4% (n=71) were receiving a generic topical non-steroid formulation, and 24.7% (n=75) were receiving advanced/branded topical products with multiple active formulations.18
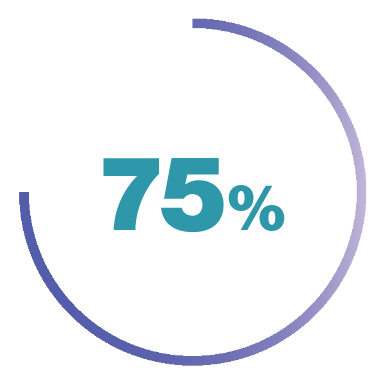
Of the 85% of patients with limited skin involvement who reported feeling “embarrassed or self-conscious because of their skin”
73% still reported feeling “embarrassed or self-conscious” because of their skin after starting their current topical therapy 2
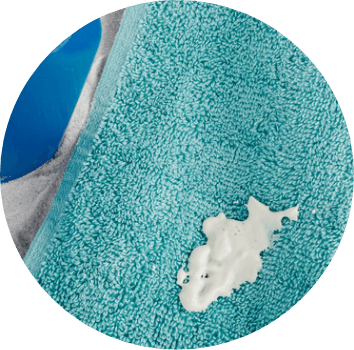
Topicals can be time-consuming, visible, messy, odorous, and can stain your patients’ skin or clothing 14
of patients report that they find topical therapy to be burdensome 3,‡‡
‡‡Based on the UPLIFT survey, a multinational online survey conducted from March 2 to June 3, 2020, including adult patients (≥18 years of age) who reported that they had been diagnosed with plaque psoriasis and/or psoriatic arthritis by a healthcare professional. 1,006 patients were surveyed in the United States.3

“A lot of these topicals are gel based or petroleum based. […] It would like wipe off or rub on your clothes, you would get stains… you’d find it on your pillow.”
- CATHERINE
~50% of patients with limited skin involvement on topicals


Patients may have difficulty effectively applying topicals to their scalp (due to hair) and to their nails (due to the nail structure and texture). 14,20
Topicals can be irritating for use in the genital areas. 21
Thicker hyperkeratotic lesions are common in patients with skin of color and may require higher potency topicals. 22

Topical steroids can lead to hypopigmentation on skin of color, which may cause additional challenges even after plaques heal. 22,23

Hair texture in patients with skin of color can pose challenges when applying topicals and treating scalp psoriasis. 24

“I had pitting in the nails and [my HCP] said that it could be indicative of psoriatic arthritis. And I was kind of in denial. […] Like, I don’t have arthritis. I’m 27 years old. What are you talking about?”
- CATHERINE
Even for psoriasis patients with limited skin involvement, underlying inflammation may remain 5,27
BSA, body surface area; IPC, International Psoriasis Council; MAPP, Multinational Assessment of Psoriasis and Psoriatic Arthritis; NPF, National Psoriasis Foundation; PsA, psoriatic arthritis.
References: 1. Lebwohl M, Ogdie A, Merola J, et al. Maui Derm Poster. 2021. 2. Gupta S, Garbarini S, Nazareth T, et al. Dermatol Ther. 2021;1-19. 3. Lebwohl M, Langely R, Paul C, et al. Dermatol Ther. 2022;12:61-78. 4. Strober B, et al. J Am Acad Dermatol. 2020;82(1):117-122. 5. Van Voorhees A, Feldman S, Lebwohl M, et al. The Psoriasis and Psoriatic Arthritis Pocket Guide. psoriasis.org/the-pocket-guide. Accessed August 15, 2023. 6. Augustin M, et al. Br J Derm. 2019; 1-8. 7. Menter A, et al. J Am Acad Derm. 2019;80(4):1029-1072. 8. Strober BE, et al. Dermatol Ther (Heidelb). 2019;9:5-18. 9. Blakely K, et al. Psoriasis: Targets and Therapy. 2016;(6):33-40. 10. Wilson FC, Icen M, Crowson CS, et al. Arthritis Rheum. 2009;61(2):233-239. 11. Kimmel GW, Lebwohl M. Psoriasis: Overview and Diagnosis. Evidence-Based Psoriasis. Updates in Clinical Dermatology. 2018;1-16. 12. National Psoriasis Foundation. psoriasis.org. Accessed July 1, 2023. 13. Dopytalska K, Sobolewski P, Błaszczak A, et al. Reumatologia. 2018;56(6):392-398. 14. Merola J, Qureshi A, Husni M. Dermatol Ther. 2018;31(3):e12589. 15. Lebwohl MG, et al. J Am Acad Dermatol. 2014;70(5):871-881.e30. 16. Van de Kerkhof PC, Reich K, Kavanaugh A, et al. J Eur Acad Dermatol Venereol. 2015;29(10):2002-2010. 17. Van Voorhees AS, Feldman SR, Lebwohl MG, et al. The Psoriasis and Psoriatic Arthritis Pocket Guide. psoriasis.org/the-pocket-guide. Accessed November 20, 2020. 18. Kaplan D, Hetherington J, Lucas J, et al. J Dermatol Treat. 2022;33(6):2844-2852. 19. Data on file, Amgen Inc. 20. Aldredge LM, Higham RC. J Dermatol Nurses Assoc. 2018;10(4):189-197. 21. Beck K, Yang E, Sanchez I, et al. Dermatol Ther (Heidelb). 2018(8):509-525. 22. Ishizuka BS, Soung J. Practical Dermatology. 2021;56-57. 23. Coondoo A, Phiske M, Verma S, et al. Indian Dermatol Online Journal. 2014;5(4):416-425. 24. Alexis A, Blackcloud P. J Clin Aesthet Dermatol. 2014;7(11):16–24. 25. Mease PJ, Armstrong AW. Drugs. 2014;74(4):423-441. 26. Armstrong A, Bohannan B, Mburu S, et al. Dermatol Ther. 2022;1-10. 27. Schafer P. Biochemical Pharma. 2012;83:1583-1590. 28. Menter A, et al. J Am Acad Dermatol. 2020;82(6):1445-1486.